Overview
Health Net Federal Services, LLC (HNFS) must verify TRICARE beneficiaries meet specific eligibility requirements before authorizing services under the Autism Care Demonstration (ACD).
Beneficiaries must meet the following eligibility requirements prior to enrollment into the ACD. HNFS may receive one or more of the following notifications indicating the beneficiary may be eligible to access services under the ACD, which will initiate the pre-enrollment process:
- Notification from a parent, Exceptional Family Member Program (EFMP) case manager, military hospital case manager, or clinic case manager
- Referral to the ACD from a referring provider
- Referral for applied behavior analysis (ABA) services from a TRICARE-authorized autism spectrum disorder (ASD)-referring and diagnosing provider
HNFS will support families for up to 180 days during pre-enrollment to help them with enrollment requirements.
Tip: View/download our process flow that walks you through the ACD nomination to first treatment authorization.
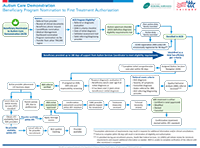
(Full text of process flow)
TRICARE Eligibility Criteria
Beneficiaries must be enrolled a TRICARE health plan to be eligible for the ACD:
- Dependents of active duty service members must register for the Extended Care Health Option (ECHO) to participate in the ACD. ECHO registration deadlines apply. Learn more on our registering for ECHO page or refer to the "Definitive Diagnosis Requirements" section below.
- Those covered by the Transitional Assistance Management Program, Continued Health Care Benefits Program, or as a foreign force member may also be eligible for the ACD.
Autism Care Demonstration Enrollment Criteria
Diagnosis of Autism Spectrum Disorder
Eligible beneficiaries must have an ASD (F84.0) diagnosis by a TRICARE-authorized primary care manager (PCM) or TRICARE-authorized ASD referring or diagnosing provider.
Diagnosis occurs under the TRICARE basic benefit. TRICARE beneficiaries nominated for the ACD must have their TRICARE-authorized ASD-diagnosing and referring provider submit either a referral or diagnostic evaluation stating a diagnosis of ASD using Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria to initiate the process for enrollment into the ACD.
The following TRICARE-authorized provider types can diagnose and submit referrals:
| PCMs |
ASD-Diagnosing Specialists |
|---|
- Pediatricians
- Pediatric family medicine physicians
- Pediatric nurse practitioners
|
- Physicians board-certified or board-eligible in:
- Developmental behavioral pediatrics
- Neurodevelopmental pediatrics
- Pediatric neurology or psychiatry
- Doctoral-level clinical psychologists
- Specific board-certified doctors of nursing practice (DNP*) who meet criteria
|
Note: Diagnoses and referrals from physician assistants and residents/students in organized health care, or other providers not having the above qualifications, will not be accepted unless the referral is cosigned by a PCM or specialized ASD-diagnosing provider in one of the approved specialties.
*DNPs credentialed as developmental pediatric providers require dual American Nurses Credentialing Center (ANCC) board certifications as either a pediatric nurse practitioner or a family nurse practitioner, and either a child psychiatric mental health nurse practitioner (PMHNP) or a child psychiatric and mental health clinical nurse specialist (PMHCNS). DNPs credentialed as psychiatric and mental health providers require a single ANCC board certification as either a PMHNP or PMHCNS.
Definitive Diagnosis Requirements
TRICARE-authorized ASD-diagnosing and referring providers must submit the following as part of the enrollment process:
- A referral or diagnostic evaluation indicating an ASD diagnosis. Eligible beneficiaries must have an ASD diagnosis by a TRICARE-authorized PCM or specialized ASD-diagnosing provider. HNFS is unable to accept a “provisional” diagnosis. The referral may or may not specify ABA services. If the original referral received by HNFS does not meet the criteria for ABA services but meets the criteria for the first component of a definitive ASD diagnosis, we will request a referral for ABA services from the referring provider once enrollment is complete.
- The date of the initial ASD diagnosis. We require, at a minimum, the year of diagnosis but will request “month/day/year” from the referring provider if not included in other submitted documentation.
- A completed DSM-5 Diagnostic Checklist. The DSM-5 Diagnostic Checklist identifies the level of support required according to DSM-5 ASD criteria. Only TRICARE-authorized ASD diagnosing and referring providers are eligible to complete the checklist. ABA providers are not permitted to complete the form. Note: The provider who completes the checklist does not have to be the same provider who completed the original diagnosis.
- Beneficiaries new to the ACD as of Oct. 1, 2021: HNFS will collect a completed DSM-5 Diagnostic Checklist from a TRICARE-authorized ASD-diagnosing or referring provider prior to enrollment and at each two-year referral cycle.
- Beneficiaries enrolled in the ACD prior to Oct. 1, 2021: HNFS will collect a completed DSM-5 Diagnostic Checklist at the next two-year referral cycle that occurs on or after Oct. 1, 2021, and at each subsequent two-year referral cycle.
- Complete results of an approved validated assessment tool (VAT).
- Beneficiaries new to the ACD as of Oct. 1, 2021: HNFS will collect the results of an approved, VAT from the TRICARE-authorized ASD-referring and diagnosing provider prior to enrollment.
- Beneficiaries enrolled in the ACD prior to Oct. 1, 2021: HNFS will collect VAT results at the next two-year referral cycle that occurs on or after Oct. 1, 2021.
- The VAT results submission is a one-time requirement.
- Any one of the following VATs meet this requirement:
- Screening Tool for Autism in Toddlers and Young Children (STAT™)
- Autism Diagnostic Observation Schedule™, Second Edition (ADOS®-2)
- Autism Diagnostic Interview – Revised (ADI-R®)
- Childhood Autism Rating Scale™, Second Edition (CARS™-2)
- Gilliam Autism Rating Scale, Third Edition (GARS-3). (Note: Also requires submission of diagnostic evaluation with documentation of diagnosing methods used to supplement the GARS-3 parent questionnaire.)
- Definitive diagnosis attestation option (ONLY for beneficiaries enrolled to the ACD prior to Oct. 1, 2021). To help meet definitive diagnosis requirements and proactively prevent gaps in care, TRICARE-authorized ASD referring and diagnosing providers have the option of submitting a Definitive Diagnosis Referring Provider Attestation for beneficiaries who entered the ACD prior to Oct. 1, 2021.
- This attestation fulfills both the DSM-5 Diagnostic Checklist and VAT eligibility requirements effective Oct. 1, 2021, for those enrolled in the ACD prior to that date.
- For this population, HNFS can accept any version of the VAT.
- Providers who prefer can submit the DSM-5 Diagnostic Checklist and the results of an approved, VAT instead of the attestation.
- Registration or provisional registration in ECHO (for active duty family members). Active duty family members must be registered in ECHO to participate in the ACD. Active duty family members not currently enrolled in ECHO will receive provisional registration for up to 90 days. During the 90 days, the beneficiary’s Defense Enrollment Eligibility Reporting System (DEERS) record will reflect a “400” eligibility code indicating the active duty family member can access the ECHO benefit and continue the process of ACD enrollment and initiating ABA services.
- Active duty family members who do not submit proof of EFMP enrollment (or a waiver, when eligible) within the 90 days will be disenrolled from ECHO and will no longer be eligible for ABA services.
- The 400 code shown in DEERS is the same indicator for provisional and registered status.
- HNFS will offer Autism Services Coordinators (non-clinical coordinators with ACD experience) to assist beneficiaries and provide family support for those who lose eligibility for ABA services between the expiration of the 90-day provisional period and registration into ECHO. If ECHO registration has not been completed after 180 days, the beneficiary will no longer be eligible for the ACD.
Autism Care Demonstration Enrollment Support
Once HNFS has verified all definitive diagnosis and enrollment criteria have been met, the beneficiary will be officially enrolled into the ACD.
HNFS' Autism Services Coordinators (non-clinical coordinators with ACD experience) can help families with pre-enrollment criteria. Beneficiaries who are not able to complete all enrollment criteria within the 180 days of support from the Autism Services Coordinator may initiate reentering the program when criteria have been met.
Note: An Autism Services Coordinator is not the same as an Autism Services Navigator (ASN). Learn more about ASNs on our Autism Services Navigators page.
Request for ACD Services