Skills to Help Manage Asthma
Skills to Help Manage Asthma
By learning and applying skills, you can have better control over your asthma and maintain control of it.
One important skill is monitoring your symptoms in a diary. Studies show that after two weeks, one's recall is less and less. If you visit the doctor and he or she asks how you have been, your perception is often based on the previous two weeks only. For example, if a month ago you had an attack due to bad weather that lasted for a while, you may not tell your doctor because you have since forgotten about it. But if you keep a log of your shortness of breath, increased wheezing or coughing and increased fatigue with minimal activity, you can report it to the doctor. Monitoring your symptoms in a diary can give your doctor a better picture of the entire time in between visits, and let him or her see how controlled your asthma has been.
- Monitor these symptoms in your diary daily:
- increased shortness of breath
- increased wheezing or coughing
- increased tiredness with minimal activity

Peak Flow Meters and Daily Monitoring
Similar to how a diabetic monitors their blood sugar, someone with asthma monitors their peak expiratory flow. A peak flow meter is a tool used to take peak flow readings, which is a measure of how fast air comes out of the lungs when you exhale forcefully after inhaling fully.
The peak flow meter is not meant to be used for diagnosing asthma, but as a monitoring device. Most importantly, it is used to give a daily forecast of your asthma so you can pretreat your asthma appropriately and avoid a visit to the emergency room. It’s important to include your peak flow readings in your symptom diary.
Benefits of Monitoring Peak Flow Measurements:
- If the doctor makes any changes in your asthma therapy, your peak flow meter can be an early indicator that the changes are working for the better or the worse. Your readings help your doctor make decisions about your treatment.
- It can alert you that your asthma symptoms are worsening and you need to start following your asthma action plan. For example, if your peak flow reading is low, it can act as an early warning system that there is a problem, sometimes before you feel symptoms. This can lead to early treatment and prevent a more severe flare-up.
- It can help you and your doctor decide if you need to adjust your daily medication.
- Peak flow monitoring can also help people who have asthma for a long time realize that their asthma is not in good control or in the first stages of an asthma flare-up. People with long-term, poorly controlled asthma can be so used to some shortness of breath, wheezing or coughing that they don’t think to use their short acting inhaler until symptoms are more severe.
When to Use a Peak Flow Meter:
1. First determine your personal best:
Your personal best is taken when you are feeling healthy and have no symptoms. It is used as a baseline to compare your daily peak flow outcomes. You can consider your personal best as 100 percent. A future reading that is 80 percent of your personal best puts you in the yellow, or caution zone on your asthma action plan. This indicates that you need to use your rescue medication per your doctor’s instruction. A future reading that is at 50 percent or lower of your personal best puts you in the red, or danger zone on your asthma action plan. This indicates that you’re in danger of a severe asthma flare-up and medical intervention is needed per your doctor’s instruction.
2. As needed for daily monitoring:
• First thing in the morning, before medications, to forecast your day
• Before medications, or two hours afterwards
• When symptoms of asthma are present
• When you are exposed to triggers
• When you have medication changes
• As directed by your doctor
How to Use a Peak Flow Meter:
- Stand in an upright position,
- Place device past the teeth,
- Breathe in deep and exhale forcefully into the device; and
- Record the best of three tries in your symptom diary.
If you don’t have one already, ask your doctor for a peak flow meter at your next appointment.
Action: Use the Daily Diary to help you monitor.

Asthma Action Plan
Everyone should work with their doctor to create a personal daily action plan. It can be symptom-based or peak-flow based. It should be available at home, school, day care, and at your work. If you have children with asthma, every caretaker should have a copy of the action plan. To make it easier to follow, the plan consists of three zones - green, yellow and red, like a stop light. The plan will describe your daily treatments, such as which medicines to take and when to take them. Using your plan will help you know when to treat right away instead of waiting to contact a doctor and will explain when you should call the doctor or go to the emergency room.
You can download a copy from the NHLBI.gov website, use the Action Plan provided below, or ask for one at your next doctor appointment.
Action:
1. Read Managing Your Asthma to learn about preventive and rescue medicines and how to complete an asthma action plan.
2. Complete your Asthma Action Plan with help from your doctor for a thorough asthma management plan. Use the Pediatric Action Plan if it is your child who has asthma.
Daily Management – Putting it all Together
By putting all of your skills together on a daily basis, you will prevent more attacks in the future. It may seem like a lot to do every day but once you work it into your routine it doesn’t take much to prevent attacks. It’s like your car: You keep an eye on the gauges and when the check engine light comes on, you take it in and have it fixed. Monitoring your peak flows and symptoms is like watching those gauges. When the light comes on, treat with the appropriate medications before it gets really bad.
Taking your daily medications is also like car maintenance: You don’t wait for it to break down on the side of the road to do an oil change, you keep up on the maintenance to assure a smooth running vehicle. You need to use your daily medications even if everything is going smoothly and you are not having asthma problems. Don’t wait for an attack to reach for your daily preventive medication.
Try to avoid triggers as much as possible without decreasing your quality of life. There are some triggers that we just can’t avoid, so avoid the ones you can. Treat early! Don’t wait until the asthma flare-up is out of your control before treating it. Treat at the first sign of an attack and you will save yourself an ER visit or three days in bed, or you'll avoid missing work or school.
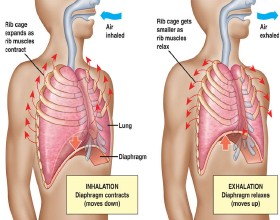
Diaphragmatic Breathing
Diaphragmatic breathing is a skill that should be practiced a lot so it can be used effectively when you have an asthma flare-up. You can also use it during exercise or when feeling stressed. It is good to practice to increase endurance of your main breathing muscle – the diaphragm. Don’t try to do it when you are feeling short of breath.
Directions:
- Sit or stand comfortably, or lie on your back with your knees supported.
- Place your hands on your belly.
- As you inhale, feel your belly push out.
- Feel your belly relax back in toward your spine as you exhale.

Pursed Lip Breathing
Pursed lip breathing is another skill to practice to help you when you are feeling short of breath.
Directions:
- Inhale slowly through your nose for two counts, feeling your stomach relax and your lower ribs expand.
- Pull your stomach muscles in as you exhale slowly for four counts through pursed lips. Purse your lips as if you are going to whistle or blow out a candle.
- Rest after three or four breaths.