Autism Care Demonstration: Subsequent Authorizations and Continuing Treatment
Overview
A Health Net Federal Services, LLC (HNFS) approval is required for applied behavior analysis (ABA) services for all beneficiaries, including those with other health insurance.
- Authorization requests must be submitted electronically and will be processed within two to five business days once all required documentation has been received.
- Submitting a request to HNFS is not a confirmation of authorization.
- ABA providers can check the status of an authorization or download a copy of the approval letter by using our Check Authorization Status tool.
Tip: View/download our process flow that walks you through reauthorizations of ABA treatment.
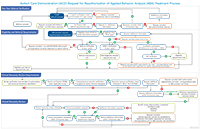
(Full text of process flow)
Step 1 – Reassessment and Treatment Plan Update
To prepare for reauthorization of care, ABA providers must complete a reassessment and treatment plan update every six months.
If continued treatment and ABA services are clinically indicated, ABA providers must submit an online request for reauthorization prior to the expiration of each six-month authorized treatment period. ABA providers can submit this as early as 60 calendar days in advance, but it must be submitted no later than 30 calendar days in advance.
HNFS requires a complete packet that meets all ACD requirements before we can conduct a clinical necessity review. Once we have received the request for continued treatment we will verify the following requirements have been met:
- TRICARE eligibility
- Autism Care Demonstration (ACD) eligibility
- Treatment plan that documents beneficiary progress and corresponding treatment recommendations demonstrating clinical necessity
- Treatment plan with beneficiary and parent/caregiver goals and engagement
- Pervasive Developmental Disorder Behavior Inventory (PDDBI) Parent and Teacher Form scores
- Current outcome measures for Vineland Adaptive Behavior Scores, Third Edition (Vineland-3); Social Responsiveness Scale, Second Edition (SRS-2); and either the Parenting Stress Index, Fourth Edition Short Form (PSI-4-SF) or Stress Index for Parents of Adolescents (SIPA)
- Individualized Education Program (IEP), when applicable
- Current two-year referral
- Current comprehensive care plan (when an Autism Services Navigator has been assigned)
Updated treatment plan
The treatment plan should be organized into the following main categories:
- Identifying Information
- Reason for Referral and Diagnosis
- Background Information
- Summary of Assessment Activities (when applicable)
- Goals and Progress Summaries
- Behavior Intervention Plans (when applicable)
- Recommendations and Units
- Updated Discharge Criteria
- Signatures
Treatment plans must include all data points and areas outlined in the TRICARE Operations Manual.
View our Treatment Plan Requirements guide to ensure the necessary requirements are included.
The treatment plan must include identification of new behavior targets, objectives, goals, and modifications based on the cumulative six-month assessment of the PDDBI and other outcome measure evaluations. Updated treatment plans also must include rationale for a lack of progress including, but not limited to:
- Regression or stagnation of outcome measure scores (for example, PDDBI, Vineland Adaptive Behavior Scales, Third Edition [Vineland-3], Social Responsiveness Scale, Second Edition [SRS-2]);
- Parent/caregiver training goals;
- Generalization; and
- Discharge planning.
The ABA supervisor should provide updates to the behavior intervention plan when applicable and update graphs or summaries for goals marking the progression of targeted skills and/or reduction of behavior excesses.
Treatment plan updates must document the number of parent/caregiver training sessions rendered over the current authorized treatment period to confirm the required minimum of six training sessions has been met. For those treatment plan updates submitted within 60 to 30 days before the end of the current authorized treatment period, if six training sessions have not occurred, the projected number of parent training sessions that will take place in the last 60 to 30 days of the current authorized treatment period must be listed to demonstrate that the minimum requirement for parent/caregiver training sessions will be met.
PDDBI Parent and Teacher Form scores
Providers are required to submit the full publisher print report or clear, legible hand-scored protocol and summary score sheet(s). Providers must label the PDDBI to distinguish which is the Parent Form and which is the Teacher Form. HNFS cannot accept PDDBI scores embedded within the treatment plan as a table. If completing the PDDBI scoring manually, include all documents related to scoring in the submission. Invalid or incomplete scoring will not be accepted. The PDDBI must include the name of the respondent and relationship to the beneficiary. The responsible ABA supervisor must complete the Teacher Form of the PDDBI. Visit our Outcome Measures page to learn more.
Parent/caregiver training and goals
An integral component of a strong clinical ABA program is engaging with parents/caregivers to teach ABA principles for teaching new skills and ensuring generalization of skills taught during ABA treatment.
- The inclusion of parent/caregiver training and goals in the treatment plan is an opportunity for the ABA provider to support parents/caregivers with implementing ABA goals outside of program hours.
- During each subsequent request for treatment, the ABA provider should outline parent/caregiver training and engagement in the ABA program. Parents/caregivers are expected to learn ABA principles, participate in ABA services being rendered in each location provided (for example, home, center/clinic), generalize mastered skills, and learn how to teach new skills and address behavior excesses across environments. The ABA provider has an important role in delivering a parent/caregiver training program that will empower families to successfully manage the diagnosis outside of program hours and long term.
Request for treatment reauthorization/recommended units
If continued ABA services are indicated, the treatment plan must specify recommendations for each Current Procedural Terminology (CPT®) code to include the location of services.
- For each relevant adaptive behavior services (ABS) CPT code, the recommendations for treatment must be submitted as units. We cannot accept other formats (hours).
- Updates to unit recommendations should be based on data analysis and beneficiary progress/lack of progress.
- Requests for units must reflect a combination of the symptom domains and levels of support required per Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria, outcome measure results, and the capability of the beneficiary to actively participate in ABA services.
- Treatment plans must include recommendations for monthly parent/caregiver training, submitted as units.
- ABA providers must render the first session of parent/caregiver training (CPT codes 97156 or 97157) within 30 calendar days of each treatment authorization.
- If parent/caregiver participation is not possible, the treatment plan must reflect the reason and mitigation efforts undertaken by the provider to resolve.
- Treatment plan updates must document the number of parent/caregiver training sessions rendered over the previous treatment period. Note: A minimum of six parent/caregiver training sessions must be conducted over a six-month authorized treatment period.
- All attempts must be made to meet this requirement and explanations included when it is not met. Failure to meet this requirement for two consecutive authorizations can result in the treatment request not being approved.
- The treatment plan must identify the location of service for each requested CPT code (home, clinic/center, school, community, and daycare).
- If CPT code 97153 is being rendered by an ABA supervisor in the school setting, rationale and explanation of short-term intervention and an IEP are required.
- Authorizations for any service performed by behavior technicians (BTs) under CPT code 97153 in the school setting will not be approved.
- ABA treatment goals performed in the school setting cannot overlap with IEP goals.
Service Locations
Please review definitions/guidelines for home, clinics/centers, daycares, school settings, and community settings on our Locations for ABA Services page.
CLINICAL NECESSITY REVIEWS
HNFS is required to perform clinical necessity reviews and clinical consultations, if applicable, on all compliant treatment authorization requests prior to issuing coverage determinations. Qualified, clinical reviewers (Board Certified Behavior Analyst® [BCBA®], Board Certified Behavior Analyst – Doctoral® [BCBA-D®]) will conduct these reviews/consultations. Please visit our Clinical Necessity Reviews page for complete details.
ABA providers may not be reimbursed for any services rendered prior to reauthorization requests being approved by HNFS.
- Submitting a request to HNFS is not a confirmation of authorization.
- Do not provide reimbursable ABA services without an approved authorization. HNFS will deny reimbursement for services performed outside the dates approved on the authorization.
- HNFS does not issue backdated authorizations. If an authorization is pended or canceled due to missing supporting documentation or an incomplete clinical necessity review (to include the consultation with the ABA supervisor or an update to a treatment plan), the authorization will be reissued from the date HNFS received all required information.
Step 2 – Referral Cycle Check
HNFS will perform a referral cycle check after receiving a request for reauthorization. If the referral cycle due date is past the date of the next reauthorization start date, HNFS will request the beneficiary obtain an updated referral prior to approval.
Since the ABA referral is valid for two years, a new referral is not required at each six-month authorization renewal period for provider changes or permanent change of station transfers within the two-year cycle.
If a new referral is required for the next two-year period, HNFS will cancel the request and notify the ABA provider and the beneficiary. Follow the instructions provided on our Referrals for ABA Services page for more information on the requirements for the referring provider to submit a new referral.
Note: For beneficiaries referred by a military hospital or clinic, please do not contact the military hospital or clinic when a new referral is required. HNFS will send correspondence to the referring provider and beneficiary.
DSM-5 Diagnostic Checklist
A completed DSM-5 Diagnostic Checklist is required at enrollment and at each subsequent two-year referral renewal cycle.* The DSM-5 Diagnostic Checklist identifies the level of support required according to DSM-5 autism spectrum disorder (ASD) criteria. Only TRICARE-authorized ASD diagnosing and referring providers are eligible to complete the checklist. ABA providers are not permitted to complete the form. Note: The provider who completes the DSM-5 Diagnostic Checklist does not have to be the same provider who completed the original diagnosis. Learn more on our Eligibility & Diagnostic Criteria page.
HNFS can accept a DSM-5 Diagnostic Checklist completed up to 180 days before the end of the referral due date.
*For beneficiaries enrolled in the program prior to Oct. 1, 2021, HNFS will collect a completed DSM-5 Diagnostic Checklist at the next two-year referral cycle that occurs on or after Oct. 1, 2021, and at each subsequent two-year referral cycle.
Step 3 – Outcome Measure Cycle Check
After the referral cycle check has been completed, HNFS will perform an outcome measure cycle check. All beneficiaries must have complete, valid outcome measure scores for HNFS to process treatment authorization requests. See Outcome Measures for complete details.
TRICARE requires ACD participants to complete and submit scores for the following outcome measures:
- PDDBI (Parent/Teacher Forms, when applicable)
- Vineland-3
- SRS-2
- Parenting Stress Index, Fourth Edition Short Form (PSI-4-SF) (0 years–12 years and 11 months) or the Stress Index for Parents of Adolescents (SIPA) Profile Form (11 years–19 years and 11 months). Similar to other outcome measures, providers submit only the
PSI-4-SF or SIPA scores (not the questions or calculations) to HNFS.
If the ABA provider has submitted the request for treatment, the treatment plan, the PDDBI Parent Form, and the IEP (when applicable) but the outcome measures remain outstanding, HNFS will contact the beneficiary to facilitate their completion by the approved provider.
Discharge, Termination and Provider Changes
Discharge: Discharge planning should occur during each reassessment, and discharge from ABA services should occur when ABA services are no longer clinically necessary.
A discharge plan should be developed between the ABA provider and the beneficiary for the short- and long-term plan to generalize mastered skills, teach new skills in the natural environment, and prepare a family for long-term management once ABA services are no longer clinically necessary.
When a beneficiary has met this criteria and is ready to begin discharge, the ABA provider can recommend a step-down in frequency, intensity and duration of services to include an increased amount of parent/caregiver training and support. ABA providers may request authorization for parent/caregiver training-only authorizations (CPT codes 97156, 97157) during the discharge process or if barriers to rendering direct ABA services prevent the active delivery of ABA services.
When the beneficiary is ready to transition out of all direct ABA service hours, and the parent/caregiver no longer needs training, the ABA provider is required to submit a discharge report to HNFS. Discharge report writing is not a billable activity. The ABA provider should notify HNFS regarding the discontinuation of services and submit the termination report electronically using the ACD ABA Discharge Report Submission request profile type.
Termination of Services and Provider Changes
In some scenarios, the termination of ABA services may be applicable, and the beneficiary or ABA provider may contact HNFS to discuss the transition of care to a new provider.
- HNFS can facilitate the transition of care to a new ABA provider, if applicable, and assist the beneficiary during this process.
- The ABA provider and/or the beneficiary should call our ACD customer service line to discuss termination from ABA services, provide a timeline for the transition and detail the justification for the termination.
- Termination from ABA services by the ABA provider cannot occur abruptly. ABA providers must provide a minimum of 45 days’ notice to both HNFS and the beneficiary prior to termination.
- ABA providers must submit discharge reports to HNFS (discharge report writing is not a billable activity) at the conclusion of treatment.
CPT® is a registered trademark of the American Medical Association. All rights reserved.