Overview
Health Net Federal Services, LLC (HNFS) performs a two-step review process consisting of an administrative review and a clinical necessity review for all authorziation requests.
Step 1 – Administrative Document Review
Before the clinical necessity review process can begin, HNFS conducts an administrative review to verify the following requirements:
- The patient’s TRICARE eligibility
- The patient’s Autism Care Demonstration (ACD) eligibility
- A valid two-year referral for ABA services and a Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition Diagnostic Checklist (DSM-5 Diagnostic Checklist) on file
- A complete treatment plan meeting all TRICARE requirements. The treatment plan must include all required sections, detail location/setting services, and have parent/caregiver and ABA supervisor signatures. Note: The ABA supervisor must submit an updated treatment plan meeting requirements at least 30 days and no more than 60 days in advance of the current authorization’s expiration for reassessment.
- Outcome measure scores and required data points (including the name/credentials of the respondent and their relationship to the beneficiary):
- Pervasive Developmental Disorder Behavior Inventory (PDDBI) Parent and Teacher Forms when applicable (completed by both the parent/caregiver and ABA supervisor),
- Vineland Adaptive Behavior Scales, Third Edition (Vineland-3),
- Social Responsiveness Scale, Second Edition (SRS-2),
AND
- Parenting Stress Index, Fourth Edition Short Form (PSI-4-SF) or Stress Index for Parents of Adolescents (SIPA)
- An Individualized Education Program (IEP) when treatment is recommended in the school setting
- A comprehensive care plan (CCP) when applicable
HNFS' administrative document review can take up to five business days. If required elements are missing or incomplete, we will notify the referring and/or treating provider and pend the request for up to 10 days to allow time for the missing information to be submitted. After 10 business days, HNFS will cancel the request. Once the requested information has been received, HNFS will repeat the administrative review and reset the review timeline.
Please note:
- We will cancel requests that do not meet ACD program eligibility (definitive diagnosis) requirements or do not include outcome measures. Processing will resume once ACD eligibility requirements have been met.
- We will not pend requests that are only missing the IEP; rather, we’ll request this during the clinical necessity review. If an IEP is not available during the clinical necessity review and school services by an ABA supervisor are being requested, additional information or consultations may be required to clarify the scope of services.
Step 2 – Clinical Necessity Review
HNFS’ clinical necessity reviews and clinical consultations are conducted by our qualified reviewers (Board Certified Behavior Analysts® [BCBA®], Board Certification Behavior Analysts – Doctoral® [BCBA-D®]) who follow a standardized review approach. Clinical necessity reviewers are also referred to as Autism Clinical Care Analysts (ACCA).
Clinical necessity reviews require a complete analysis of the treatment plan, including assessment results, recommended goals and target areas, parent/caregiver training goals, outcome measure scores, and dose recommendations. After completing the clinical necessity review, if necessary, HNFS will have a clinical consultation (a live, phone review of the treatment plan), with the ABA supervisor before issuing a coverage determination.
ACCAs ensure treatment plans coincide with the most appropriate level of care for beneficiaries and take into consideration:
- Level of clinical support (including review of outcome measures and progress over time)
- Treatment plan
- Efficacy of treatment implementation
- Dose response (intensity, frequency, duration)
- Duration of services and individualized discharge planning
- Other rendered services
ACCAs also use clinical necessity reviews to identify treatment exclusions and any missing required treatment plan elements, as well as dose recommendations, level of impact, duration of services, response to treatment, and other evidence-based treatments.
The ACCA evaluates all clinical documentation including but not limited to:
- Baseline data, progress summaries and ongoing data collection
- Recommended goals
- Parent/caregiver training goals, treatment participation, and generalization of skills
- Behavior intervention plans
- Outcome measure scores
- Exclusions (For detailed information, visit our Exclusions page and review TRICARE Operations Manual, Chapter 18, Section 4.)
- Required treatment plan information (Refer to our Treatment Plan Requirements guide for more information.)
- Beneficiary name
- Date of birth
- Initial assessment date
- Date of reassessment
- Subscriber Department of Defense [DOD] Benefits Number [DBN] or Social Security number [SSN]
- Referring provider information
- Diagnostic severity level
- Date of diagnosis
- Comorbid and medication information
- School and other services treatment hours
- Total number of years receiving ABA
- Location of services, etc.
- Individualized discharge plans and criteria
- Current Procedural Terminology (CPT®) code recommendations. For example:
- CPT 97158 is reviewed for which goals will be targeted and the necessary generalization or skill sets required for the beneficiary to fully benefit from a group format for treatment.
- Code recommendations follow appropriate format: 97153 recommended weekly, 97155, 97156, 97157, 97158 recommended monthly and 97151, 99366, 99368 recommended per treatment period.
- Community location recommendations are reviewed for specific locations, provider type and target goals specific to each proposed location. Service recommendations must be focused and in accordance with the requirements of the ACD.
- IEP review for school location recommendations:
- School locations requests are reviewed for overlap between IEP and ABA program goals, amount of services and goals specific to the school location, as well as proposed limited durations of the school based treatment by the ABA supervisor.
Once the clinical necessity review is complete, the ACCA will either make a coverage determination, request additional information or clarification and/or request a clinical consultation with the ABA supervisor. Refer to our ACD Evaluating Treatment and Outcome Measure Progress guide for more information on clinical necessity reviews.
The clinical necessity review can take up to five business days. If required elements are missing or exclusions are present, HNFS will notify the treating provider and pend the request for up to 10 days to allow time for the requested modifications to be submitted. After 10 business days, HNFS will cancel the request. Once submitted, we will repeat the clinical review and reset the review timeline.
Clinical Consultation and/or Additional Documentation
HNFS may require consultations with the responsible, treating ABA supervisor to address and resolve areas regarding:
- Clinical necessity,
- Exclusions, and/or
- Other areas that may require more complex discussion to resolve.
Treatment plans that require modification must be resubmitted to HNFS.
- For resubmissions of treatment plans only (additional information requests): ABA providers will have 10 business days to submit an updated treatment plan. Areas requested for modification or addition will be listed in a faxed communication and include instructions on how to resubmit. Once received, we will conduct a second clinical necessity review and, as long as the request has been made compliant, we will make a coverage determination within five business days.
Note: If the updated treatment plan still does not meet ACD guidelines, HNFS will notify the provider and beneficiary via fax and/or during the clinical necessity consultation, and the timeline will reset.
- For clinical consultations in addition to updated treatment plans: HNFS will attempt to contact the treating ABA supervisor by the fifth day of the clinical necessity review. We will pend the request for up to 10 days to allow time for a meeting to be scheduled and conducted if initial contact has not been made. It’s important ABA supervisors respond promptly to our requests for consultations. After the clinical consultation has occurred, the ABA provider will have up to 10 business days to submit an updated treatment plan. Once received, a second clinical necessity review will be conducted and, as long as the request has been made compliant, we will make a coverage determination within five business days. If we are unable to connect with the ABA provider to schedule the consultation and/or do not get the treatment plan in a timely manner, we will cancel the request and resume processing once these actions have been fulfilled.
Processing Timelines
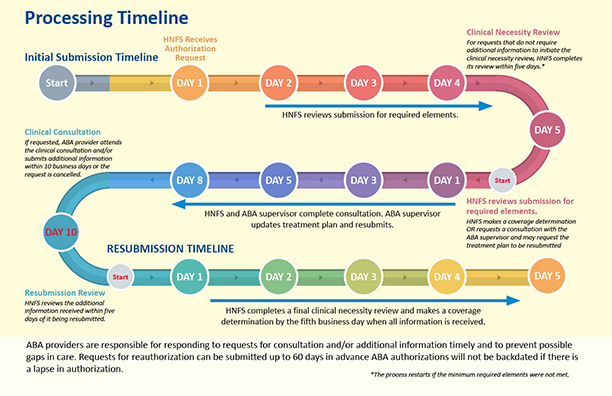
- HNFS will complete an administrative document review of the request for authorization within two to five business days of receipt by the ABA provider. The administrative review includes:
- Verification of eligibility
- Verification ACD program requirements are met
- Verification of a valid referral
- Verification of a comprehensive care plan (beneficiaries with Autism Services Navigators only)
- Verification of a complete and valid PDDBI (parent form/teacher form, as applicable)
- Verification of a complete and valid Vineland-3, SRS-2 and PSI-4-SF/SIPA
- Verification of minimum treatment plan requirements (i.e., location of services, etc.)
- HNFS will complete the administrative review (if compliant with items listed above), the clinical necessity review, and send correspondence by the fifth business day.
- If there are no changes to the treatment plan, HNFS will complete a coverage determination and send correspondence by the fifth business day.
- If a provider consultation is required, HNFS will attempt to contact the treating ABA supervisor by the fifth business day. If no contact has been made, a request to meet within the next 10 days will be faxed to the ABA supervisor. HNFS will cancel the request for authorization if the consultation has not been completed within 10 business days. The treating ABA supervisor will need to complete the consultation and resubmit the treatment plan and/or additional information for a second review for coverage determination.
- If additional information is required, HNFS will notify the treating ABA supervisor, either via a faxed letter or during a provider consultation, that modifications to the treatment plan must be completed. The ABA supervisor has up to 10 business days to resubmit the treatment plan with modifications. Once received, HNFS will complete the clinical necessity review on the now complete treatment plan within five business days for a coverage determination.
- Responding to requests for consultation and/or additional information in a timely manner is the ABA supervisor’s responsibility and helps to prevent potential gaps in care. HNFS will not issue any backdated or retro authorizations under any circumstances. The treating ABA provider is encouraged to submit the request for reauthorization up to 60 days in advance to allow for the review process, consultation process and re-review, if necessary.
Authorization Codes and Determination Reasons
Log in to our secure provider portal to check authorization status. Reference the printable Authorization Codes & Determination Reasons guide to better understand status codes and determination reasons.
Key Points
Providers must have an approved authorization from HNFS (with an authorization number) before rendering ABA services.
- Submitting a request to HNFS is not a confirmation of authorization.
- Do not provide ABA services without an approved authorization. HNFS will deny reimbursement for services performed outside the dates approved on the authorization.
- Subsequent authorizations for continuing treatment can be submitted up to 60 days in advance and no less than 30 days in advance of the current authorization's expiration.
- HNFS does not issue backdated authorizations. If an authorization is pended or canceled due to missing supporting documentation or an incomplete clinical necessity review (to include the consultation with the ABA supervisor or an update to a treatment plan), the authorization will be re-issued from the date HNFS receives all required information.
Definition and Guidelines
- Clinical necessity review: All treatment requests are reviewed for clinical necessity prior to authorization and may include requests for additional information and clinical consultation, and/or require modifications to treatment plans.
- Clinical necessity consultation: A live phone review of the treatment plan with the ABA supervisor to discuss programming, outcome measures, exclusions, etc. Clinical necessity consultations will occur with all initial treatment plan submissions and as needed for ongoing treatment requests.
- Late reauthorization request: ABA providers who submit reauthorization requests less than 30 calendar days from the expiration date of the current authorization are at risk for non-payment, should the existing authorization expire before HNFS approves the renewal request.
- Requests for authorization submission process: Submit all requests for authorization of care to HNFS using our online authorization submission tools.
- Requests for reauthorization: If continued services are clinically indicated, prior to the expiration of each six-month authorized treatment period (as early as 60 calendar days in advance but no later than 30 calendar days in advance), the ABA provider must submit a reauthorization for ABA services.
- Treatment plan: A written document outlining the ABA supervisor’s plan of care for TRICARE beneficiaries receiving ABA services.
Tip: View/download our process flow that walks you through ACD clinical necessity review.

(Full text of process flow)